Why Masks Don’t Work And How to Advocate for Logic in the Time of COVID-19
Many of you have asked for resources on how to make your voice heard in this increasingly strange time we are all living in. Whether approaching an employer, school board or a business that you frequent about your concerns with illogical policies, feel free to use these resources as a template.
Ali’s Letter to Stella’s School
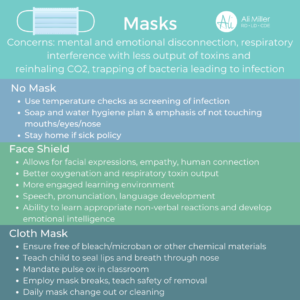
General breakdown of why masks don’t work:
1. They provide a false sense of security and people misuse them driving more potential for infection. The warm vapor of your breathing when wearing a mask pushes vapor to your eyes driving more likelyhood of touching your eyes which can spread contagion. Essential workers often wear them into the restroom and then touch their masks as they take your food order, oral-fecal contamination risk!
2. They interfere with respiratory function and your immune systems regulation as a barrier defense. You are not able to exhale fully to expel any potential pathogen that you may have conducted this can push viral load deeper into pulmonary system.
3. They can drive excessive epinephrine and cortisol as an anxiety and stress response, the shallow rapid breath mimics sympathetic nervous system response which can drive stress chemical release. The individual may experience palpable anxiety and panic. Note: these compounds when released in excess hinder the function of your immune system!
4. Asymptomatic carriers are very unlikely to spread infection, per WHO June 8th 2020, the recommendation is back to if sick stay at home, the masks merely represent fear, control, and compliance.
5. They create separation and dehumanize us. Especially in the constructs of education and connection with children who are very low risk for COVID mortality but are vulnerable for fear, shame, depression, and mental health. CDC states ages 10-34 the number 2 cause of death is suicide!
Becki’s Letter To the Texas Farmers Market
Attn: Texas Farmers Market Executive Director and Market Manager(s)
To Whom it May Concern,
I am a patron of the Mueller Farmers Market and Registered Dietitian working in the field of Integrative and Functional Medicine. I am reaching out to express my concerns with the current requirement of farmer’s market customers to wear a mask or facial covering.
As a former farmers market manager in Houston for several years, I can understand that there is an enormous amount of political pressure on a large non-profit organization such as yours to enforce sanitation and hygiene measures at all times, not just during a pandemic. I also understand from experience that vendor burnout rates are high and that consistent foot traffic is essential for market survival. My concern is that mandated masks are misguided and may ultimately be doing more harm than good to the viability of the market and to wearers both vendor and customer alike, possibly posing higher health risks due to misuse.
The market is held in an outdoor space and from what I have seen over the past several weeks, there is ample space for all customers to practice the recommended 6 feet of social distancing especially with the current line management and significantly decreased customer capacity. The very CDC and City of Austin guidelines that you cite on your website’s COVID-19 information tab do not require masks while outdoors and able to maintain 6 feet of social distance.
What’s more, requiring masks for entry excludes individuals who may not be able to wear them due to increased risk to their mental or physical health such as those with anxiety disorders, claustrophobia or medical conditions that hinder their breathing, as well as those with hearing impairment who rely on lipreading as a form of communication.
The outdoor locale of your market puts you at a significant advantage already for reduced viral transmission and pathogenicity as we have seen data out of the US Department of Homeland Security that demonstrates UV light exposure along with temperatures above 70-75 degrees and 20% humidity to decrease the half-life of SARS COV-2 virus in both air and on surfaces. (1)
What’s more, cloth masks are ineffective at blocking viral transmission. In a metaanalysis of 54 studies, it was concluded that cloth masks showed no evidence of protection against viral pathogens and might facilitate transmission of pathogens when used repeatedly without sterilization (2). Emerging evidence specific to the SARS-COV-2 virus shows that neither cloth nor surgical masks limit transmission of the virus during coughing from infected patients—one study of infected patients showed viral dissemination both inside and outside the mask (3).
I have personally observed while shopping at the farmers market over the past several weeks some concerning trends of user error while wearing cloth masks. Masks are meant to be worn in a medical or surgical setting and even then, they are recommended for short term use to be changed every two hours or between patients. Using the same mask through the duration of the market that has likely not been washed and sanitized (possibly for several days or even weeks) increases risk to both the wearer and others around them.
Wearing masks, especially in the oppressive Texas heat, causes users to actually touch their faces more frequently, fidget with masks, and wipe their eyes more often which is concerning for transmission of disease especially in the setting of a food establishment. To further this concern of user error, I have observed food vendors going back and forth to the restroom wearing the same masks which is a major concern for spread of foodborne illness including e. coli, salmonella and other pathogens.
Masks themselves may also increase risk of infection to the wearer as when an individual is infected with a respiratory virus, they expel virus with each breath. Wearing a mask in these individuals will raise the concentration of the virus in lungs and nasal passages. (4) The practice of mask wearing as a way to protect the vulnerable from asymptomatic carriers is also being disproven as those who are asymptomatic are not likely to transmit the virus. (5)
From the New England Journal of Medicine on May 21, 2020: “We know that wearing a mask outside health care facilities offers little, if any, protection from infection. Public health authorities define a significant exposure to Covid-19 as face-to-face contact within 6 feet with a patient with symptomatic Covid-19 that is sustained for at least a few minutes (and some say more than 10 minutes or even 30 minutes). The chance of catching Covid-19 from a passing interaction in a public space is therefore minimal. In many cases, the desire for widespread masking is a reflexive reaction to anxiety over the pandemic.” (6)
Per the latest information from the CDC, the best estimate of case fatality rate (CFR) in COVID-19 has decreased to .4% and may be as low as .26% across all ages. (7) I urge you to weigh this extremely low fatality rate against all of the potential issues of mask wearing especially in the context of an outdoor food establishment serving a largely health-conscious population that is already taking proactive measures of immune support just by shopping at your farmers market and a vendor base that is well-versed on proper sanitation and hygiene for disease prevention.
At best, masks are likely just blocking absorption of Vitamin D via the skin which has been shown effective in enhancing the immune system and appears to play a role in decreasing COVID-19 mortality rates. (8) At worst, they may actually be increasing risk of viral and bacterial transmission including foodborne illness to vendors and customers alike as well as creating an environment of heightened anxiety and an unsustainable future for your organization.
As a concerned citizen who would like to continue to patronize your farmers market, I implore you to reconsider the mandate of masks and allow customers to have autonomy and choice around whether or not to continue to wear them.
Thank you for your time and consideration.
Respectfully,
Becki O’Brien Yoo, MS, RD, LD
References
- DHS S&T Research & Development Response to SARS-CoV-2 https://www.dhs.gov/sites/default/files/publications/panthr_covid-19_fact_sheet_42420.pdf
- Offeddu, V., Yung, C.-F., Low, M., & Tam, C. (2016). Effectiveness of masks and respirators against respiratory infections in healthcare workers: A systematic review and meta-analysis. International Journal of Infectious Diseases, 53, 27. https://pubmed.ncbi.nlm.nih.gov/29140516/
- Seongman Bae, MD, et. al., Effectiveness of Surgical and Cotton Masks in Blocking 5. SARS-CoV-2: A Controlled Comparison in 4 Patients, Annals of Internal Medicine, 6 April 2020, https://doi.org/10.7326/M20-1342
- Coronavirus: Face masks could increase risk of infection, medical chief warns https://www.independent.co.uk/news/health/coronavirus-news-face-masks-increase-risk-infection-doctor-jenny-harries-a9396811.html
- Gao, Ming et al. A study on infectivity of asymptomatic SARS-CoV-2 carriers. Respiratory medicine, vol. 169 106026. 13 May 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7219423/
- Michael Klompas, M.D., M.P.H., et al. Universal Masking in Hospitals in the Covid-19 Era, New England Journal of Medicine, 21 May 2020 https://www.nejm.org/doi/full/10.1056/NEJMp2006372?query=TOC
- Covid-19 Pandemic Planning Scenarios https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html
- Northwestern University. Vitamin D levels appear to play role in COVID-19 mortality rates: Patients with severe deficiency are twice as likely to experience major complications. ScienceDaily, 7 May 2020. sciencedaily.com/releases/2020/05/200507121353.htm
Additional list of mask research references to share with your employer or school:
1. bin-Reza F et al. The use of mask and respirators to prevent transmission of influenza: A systematic review of the scientific evidence. Resp Viruses 2012;6(4):257-67.
2. Zhu JH et al. Effects of long-duration wearing of N95 respirator and surgical facemask: a pilot study. J Lung Pulm Resp Res 2014:4:97-100.
3. Ong JJY et al. Headaches associated with personal protective equipment- A cross-sectional study among frontline healthcare workers during COVID-19. Headache 2020;60(5):864-877.
4. Bader A et al. Preliminary report on mask induced deoxygenation during major surgery. Neurocirugia 2008;19:12-126.
5. Shehade H et al. Cutting edge: Hypoxia-Inducible Factor-1 negatively regulates Th1 function. J Immunol 2015;195:1372-1376.
6. Westendorf AM et al. Hypoxia enhances immunosuppression by inhibiting CD4+ effector T cell function and promoting Treg activity. Cell Physiol Biochem 2017;41:1271-84.
7. Sceneay J et al. Hypoxia-driven immunosuppression contributes to the pre-metastatic niche. Oncoimmunology 2013;2:1 e22355.
8. Blaylock RL. Immunoexcitatory mechanisms in glioma proliferation, invasion and occasional metastasis. Surg Neurol Inter 2013;4:15.
9. Aggarwal BB. Nucler factor-kappaB: The enemy within. Cancer Cell 2004;6:203-208.
10. Savransky V et al. Chronic intermittent hypoxia induces atherosclerosis. Am J Resp Crit Care Med 2007;175:1290-1297.
11. Baig AM et al. Evidence of the COVID-19 virus targeting the CNS: Tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci 2020;11:7:995-998.
12. Wu Y et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behavior, and Immunity, In press.
13. Perlman S et al. Spread of a neurotropic murine coronavirus into the CNS via the trigeminal and olfactory nerves. Virology 1989;170:556-560.